
Unveiling the Shocking Truth: What Kills Sperm in the Female Body?
What Kills Sperm in the Female Body: Welcome to the fascinating world of sperm and its incredible journey within the female body! In this article, we delve deep into the intricacies of sperm survival, exploring the various factors that influence their viability in the female reproductive tract.
Join us as we unravel the mysteries surrounding sperm, from their humble beginnings in the male reproductive system to their remarkable quest towards fertilization. Throughout this journey, we’ll discuss the production of sperm, their lifespan, and the challenges they face as they navigate through the female reproductive tract.
Get ready to uncover the secrets behind what kills sperm in the female body, as we explore the impact of pH levels, cervical mucus consistency, and the immune system response on sperm viability. We’ll debunk common misconceptions and shed light on the influence of lifestyle factors such as diet, exercise, and stress management on sperm health.

Throughout this exploration, we’ll also delve into the effects of medical conditions such as sexually transmitted infections, hormonal imbalances, and structural abnormalities on sperm quality. By the end of this article, you’ll gain valuable insights into promoting sperm health and fertility through healthy lifestyle choices and proactive measures.
So, let’s embark on this enlightening journey together, as we unravel the secrets of sperm survival in the female body and empower ourselves with the knowledge to optimize fertility outcomes.
Understanding Sperm – What Kills Sperm in the Female Body
Before we dive into the intricacies of sperm, let’s take a moment to appreciate the remarkable role these tiny cells play in human reproduction. Sperm, often referred to as the “seed of life,” are the microscopic agents of fertilization, responsible for the transmission of genetic material from male to female. Now, let’s explore the fascinating world of sperm in more detail.
1. What are Sperm?
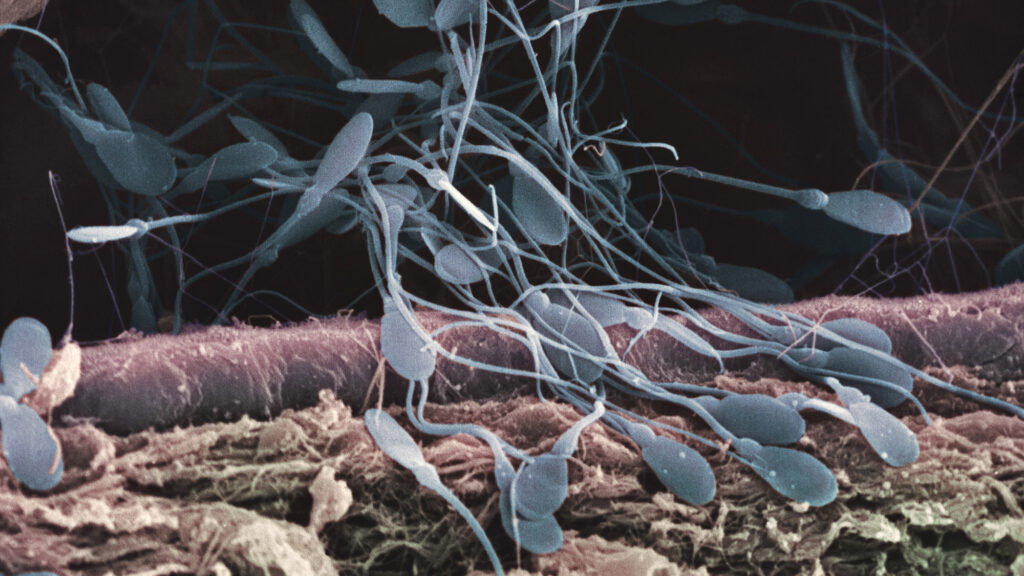
Sperm, the male reproductive cells, are marvels of nature, finely crafted for the singular purpose of fertilizing the female egg. These tiny, tadpole-like structures possess a head containing the nucleus, which houses the genetic material, and a long tail, enabling them to swim towards the egg with remarkable agility. Each sperm carries the genetic blueprint necessary for the creation of a new life, making them essential components of human reproduction.
2. Production of Sperm
The production of sperm, known as spermatogenesis, is a complex process that takes place within the seminiferous tubules of the testes. Under the influence of hormones such as testosterone, immature germ cells undergo a series of divisions and transformations, eventually maturing into fully functional spermatozoa. This intricate process requires precise regulation and coordination to ensure the continuous production of millions of sperm throughout a man’s reproductive years.
3. Lifespan of Sperm
Contrary to popular belief, sperm do not have an indefinite lifespan within the male body. Once produced, sperm undergo a series of changes as they journey through the male reproductive tract, culminating in either ejaculation or natural degradation and reabsorption. While some sperm may survive for several days within the female reproductive tract, the majority have a relatively short lifespan, highlighting the importance of timing in reproductive success.
As we unravel the mysteries of sperm production and lifespan, we gain a deeper appreciation for the intricate processes that underlie human reproduction. Join us as we continue our exploration into the journey of sperm within the female body and uncover the factors that influence their survival and viability.
Journey of Sperm in the Female Body
Before sperm can fulfill their mission of fertilizing the female egg, they must embark on a remarkable journey through the intricate terrain of the female reproductive tract. This journey, fraught with challenges and obstacles, is essential for the successful transmission of genetic material and the initiation of new life. Let’s delve into the fascinating voyage of sperm within the female body.
1. Passage through the Female Reproductive Tract
Upon ejaculation, millions of sperm are propelled into the female reproductive tract, beginning their arduous journey towards the awaiting egg. The first hurdle they encounter is the cervix, the narrow opening at the lower end of the uterus. Here, sperm must navigate through the cervical canal, which may present a formidable barrier due to its acidic environment and thick mucus consistency. Only the most resilient sperm can penetrate this initial obstacle and continue their ascent towards the fallopian tubes.
2. Challenges Along the Way
As sperm traverse the female reproductive tract, they face a myriad of challenges that threaten their survival and motility. The acidic environment of the vagina, designed to protect against infections, can be hostile to sperm, necessitating rapid movement to reach the more hospitable conditions of the fallopian tubes. Additionally, the presence of immune cells within the female reproductive tract poses another challenge, as sperm must evade detection and destruction by the body’s immune system.
As we follow the journey of sperm through the female body, we gain a deeper understanding of the remarkable resilience and adaptability of these microscopic cells. Join us as we explore the factors that influence sperm viability and survival, shedding light on the intricate mechanisms that underlie human reproduction.
Factors Affecting Sperm Viability in the Female Body
Before sperm can successfully fertilize the egg within the female reproductive tract, they must contend with various environmental factors that can profoundly impact their viability and motility. The delicate balance of pH levels, the consistency of cervical mucus, and the immune system response all play crucial roles in shaping the conditions for fertilization. Let’s explore how these factors influence the journey of sperm within the female body.
1. pH Levels
The pH levels within the female reproductive tract play a pivotal role in creating an environment conducive to sperm survival and motility. The vagina, for example, maintains an acidic pH to inhibit the growth of harmful bacteria and pathogens. However, this acidic environment can pose challenges for sperm, as it may impair their motility and viability. As sperm progress towards the fallopian tubes, they encounter a more alkaline environment, which is essential for their continued survival and eventual fertilization of the egg.
2. Cervical Mucus
Cervical mucus, produced by the cervix throughout the menstrual cycle, serves as a dynamic barrier that regulates the passage of sperm into the uterus and fallopian tubes. The consistency of cervical mucus varies depending on the stage of the menstrual cycle, with changes influenced by hormonal fluctuations. During ovulation, cervical mucus becomes thin and stretchy, facilitating the passage of sperm towards the awaiting egg. In contrast, during other phases of the menstrual cycle, cervical mucus may thicken, creating a more formidable barrier that sperm must overcome.
3. Immune System Response
The female reproductive tract is equipped with an intricate immune system that serves to protect against infections and foreign invaders. While this immune response is essential for maintaining reproductive health, it can also pose challenges for sperm survival. Immune cells within the female reproductive tract may recognize sperm as foreign entities and mount an immune response, leading to the destruction of sperm cells. Additionally, conditions such as autoimmune disorders or inflammation can further exacerbate immune-related challenges for sperm.
As we unravel the complexities of the female reproductive environment, we gain valuable insights into the factors that influence sperm viability and fertilization. Join us as we continue our exploration, delving deeper into the impact of lifestyle factors, medical conditions, and other variables on sperm health and fertility.
Common Misconceptions about Sperm Survival
Before we delve into the intricacies of sperm survival, it’s essential to address some common misconceptions that surround this topic. Despite widespread beliefs, certain myths persist regarding the viability of sperm outside the body and the influence of lubricants on sperm motility. Let’s dispel these myths and gain a clearer understanding of the factors that truly impact sperm survival.
1. Survival Outside the Body
One of the most prevalent misconceptions about sperm is the belief that they can survive for extended periods outside the male body. While it’s true that sperm can remain viable for a short time after ejaculation, their lifespan outside the body is limited. Factors such as temperature, pH levels, and exposure to air can quickly degrade sperm quality, rendering them incapable of fertilizing an egg. Contrary to popular belief, the chances of sperm surviving on surfaces or in fluids outside the body are minimal, highlighting the importance of timing and direct transfer during sexual activity for successful fertilization.
2. Influence of Lubricants
Another common misconception relates to the influence of lubricants on sperm motility and viability. Many individuals use lubricants during sexual activity to enhance comfort and pleasure, but not all lubricants are sperm-friendly. Some lubricants may contain ingredients that can impair sperm motility or damage sperm cells, reducing their chances of reaching the egg. It’s essential to choose sperm-friendly lubricants or opt for alternatives such as pre-seed lubricants specifically designed to support sperm survival and fertility.
As we debunk these misconceptions, we gain a clearer understanding of the factors that truly impact sperm survival and fertility. Join us as we continue our exploration, unraveling the complexities of sperm health and the female reproductive environment to empower individuals with knowledge and clarity on their fertility journey.
Impact of Lifestyle on Sperm Health
Before delving into the intricate interplay between lifestyle factors and sperm health, it’s crucial to recognize the profound impact that our everyday choices can have on reproductive outcomes. From diet and exercise to stress management, various aspects of lifestyle play pivotal roles in shaping sperm quality and fertility. Let’s explore how adopting healthy habits can nurture fertility and promote optimal sperm health.
1. Diet and Nutrition
The old adage “you are what you eat” holds true when it comes to sperm health. A balanced and nutritious diet rich in essential vitamins, minerals, and antioxidants can provide the building blocks necessary for sperm production and function. Incorporating foods high in antioxidants, such as fruits, vegetables, nuts, and seeds, can help protect sperm from oxidative stress and DNA damage. Conversely, a diet high in processed foods, saturated fats, and sugars may negatively impact sperm quality and fertility. By prioritizing nutrient-dense foods and maintaining a healthy weight, individuals can support optimal sperm health and enhance their chances of conception.
2. Exercise and Physical Activity
Regular physical activity not only benefits overall health but also plays a significant role in promoting sperm health and fertility. Engaging in moderate exercise can help maintain hormonal balance, improve blood flow to the testes, and regulate body weight—all of which contribute to optimal sperm production and motility. However, excessive or intense exercise may have the opposite effect, potentially leading to hormonal imbalances and reduced sperm quality. Finding a balance that incorporates regular, moderate exercise into one’s routine can help support sperm health and fertility outcomes.
3. Stress Management
Chronic stress can take a toll on reproductive health, impacting hormone levels, sperm production, and sexual function. High levels of stress hormones such as cortisol can disrupt the delicate balance of the reproductive system, leading to decreased sperm quality and fertility. Incorporating stress-reducing techniques such as mindfulness, meditation, yoga, or deep breathing exercises can help mitigate the negative effects of stress on sperm health. Prioritizing self-care and finding healthy coping mechanisms for stress can contribute to overall well-being and fertility.
As we navigate the intricate relationship between lifestyle choices and sperm health, it becomes evident that small changes can have a significant impact on fertility outcomes. By adopting healthy habits, individuals can empower themselves to take control of their reproductive health and enhance their chances of conceiving naturally. Join us as we delve deeper into the impact of lifestyle factors on sperm health and explore strategies for optimizing fertility.
Medical Conditions and Their Effects on Sperm
Before delving into the specific medical conditions that can affect sperm health, it’s essential to recognize the significant role that underlying health issues can play in fertility outcomes. From sexually transmitted infections to hormonal imbalances and structural abnormalities, various medical conditions can impact sperm production, quality, and motility. Understanding these conditions and their effects on sperm is crucial for individuals seeking to optimize their fertility journey. Let’s explore how medical conditions can influence sperm health and fertility.
1. Sexually Transmitted Infections (STIs)
Sexually transmitted infections (STIs) can have detrimental effects on sperm health and fertility. Infections such as chlamydia, gonorrhea, and syphilis can cause inflammation and damage to the reproductive organs, leading to reduced sperm production and motility. Additionally, certain STIs can result in scarring or blockages within the reproductive tract, hindering the passage of sperm. Prompt diagnosis and treatment of STIs are essential for minimizing their impact on sperm health and fertility outcomes.
2. Hormonal Imbalances
Hormonal imbalances can disrupt the delicate hormonal regulation necessary for optimal sperm production and function. Conditions such as hypogonadism, thyroid disorders, and pituitary gland abnormalities can affect hormone levels, leading to decreased sperm production and quality. Imbalances in testosterone, follicle-stimulating hormone (FSH), luteinizing hormone (LH), and other hormones can interfere with spermatogenesis and impair fertility. Addressing underlying hormonal imbalances through medication or hormonal therapy may help restore normal sperm production and improve fertility outcomes.
3. Structural Abnormalities
Structural abnormalities within the male reproductive tract can hinder the passage of sperm and impair fertility. Conditions such as varicocele, a swelling of the veins within the scrotum, can create heat buildup and disrupt sperm production. Other structural abnormalities, such as blockages in the vas deferens or abnormalities in the shape of the reproductive organs, can also impede the release and transport of sperm. Surgical interventions or assisted reproductive techniques may be necessary to address structural abnormalities and optimize fertility.
By understanding the impact of medical conditions on sperm health and fertility, individuals can take proactive steps to address underlying health issues and optimize their chances of conception. Join us as we delve deeper into the effects of medical conditions on sperm health and explore strategies for managing and overcoming these challenges on the path to parenthood.
Tips for Promoting Sperm Health – What Kills Sperm in the Female Body

Before delving into specific tips for promoting sperm health, it’s essential to recognize the pivotal role that lifestyle choices play in shaping reproductive outcomes. From diet and exercise to avoiding harmful substances and maintaining regular sexual activity, various habits can influence sperm production, quality, and motility. By adopting positive lifestyle choices, individuals can empower themselves to take control of their reproductive health and optimize their fertility journey. Let’s explore how these tips can promote sperm health and enhance fertility outcomes.
1. Healthy Lifestyle Choices
Making healthy lifestyle choices is essential for promoting optimal sperm health and fertility. A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats provides essential nutrients that support sperm production and function. Regular exercise helps maintain hormonal balance, improves blood flow to the testes, and supports overall reproductive health. Additionally, managing stress levels, getting enough sleep, and avoiding excessive alcohol and tobacco use can further enhance sperm quality and fertility.
2. Avoiding Harmful Substances
Exposure to harmful substances can have detrimental effects on sperm health and fertility. Tobacco smoke, for example, contains toxins that can damage sperm DNA and impair sperm motility. Similarly, excessive alcohol consumption can disrupt hormonal balance and decrease sperm production. Other substances, such as illicit drugs and environmental toxins, can also negatively impact sperm quality and fertility. Avoiding exposure to these harmful substances is essential for preserving sperm health and optimizing fertility.
3. Regular Sexual Activity
Maintaining regular sexual activity is crucial for promoting sperm health and maximizing fertility potential. Frequent ejaculation helps prevent the buildup of old or damaged sperm and ensures the continuous production of healthy sperm. Additionally, timing intercourse around the woman’s fertile window—typically during ovulation—can increase the likelihood of conception. Open communication with your partner about sexual frequency and timing can help ensure that you’re maximizing your chances of conceiving naturally.
By incorporating these tips into your daily routine, you can promote optimal sperm health and enhance your fertility journey. Join us as we delve deeper into the impact of lifestyle factors on sperm health and explore additional strategies for maximizing fertility outcomes.
Conclusion – What Kills Sperm in the Female Body
What Kills Sperm in the Female Body: As we conclude our exploration into the intricate world of sperm health and fertility, it’s clear that understanding the factors that influence reproductive outcomes is paramount for individuals seeking to conceive. From the remarkable journey of sperm within the female body to the impact of lifestyle choices and medical conditions on sperm health, we’ve delved deep into the complexities of human reproduction.
Throughout this journey, we’ve uncovered the secrets of sperm survival, debunked common misconceptions, and explored strategies for promoting optimal sperm health. We’ve discussed the importance of maintaining a healthy lifestyle, avoiding harmful substances, and managing stress to support sperm production and fertility. We’ve also highlighted the role of medical conditions such as sexually transmitted infections, hormonal imbalances, and structural abnormalities in shaping reproductive outcomes.
As individuals, armed with knowledge and empowered by understanding, we have the ability to take control of our reproductive health and maximize our chances of conceiving naturally. By adopting positive habits, seeking medical guidance when necessary, and maintaining open communication with our partners, we can navigate the path to parenthood with confidence and clarity.
In closing, let us embark on this journey with determination and optimism, knowing that with each positive choice we make, we bring ourselves one step closer to realizing our dreams of parenthood. Together, let’s embrace the possibilities and embark on this incredible adventure with hope and resilience.
FAQs – What Kills Sperm in the Female Body
What factors can affect sperm count?
Several factors can influence sperm count, including lifestyle choices, medical conditions, and environmental factors. Poor diet, obesity, smoking, and excessive alcohol consumption can all contribute to lower sperm counts. Additionally, exposure to environmental toxins such as pesticides, heavy metals, and radiation can negatively impact sperm production. Medical conditions such as hormonal imbalances, infections, and structural abnormalities within the reproductive system can also affect sperm count.
Does age impact sperm quality?
Yes, age can impact sperm quality. As men age, the quality and quantity of their sperm may decline. Older men may experience a decrease in sperm motility and an increase in DNA damage within sperm cells. Additionally, advanced paternal age has been associated with an increased risk of genetic abnormalities in offspring.
Can certain medications affect sperm production?
Yes, certain medications can affect sperm production. Medications such as chemotherapy drugs, anabolic steroids, and testosterone replacement therapy can suppress sperm production and reduce sperm count. Additionally, some medications used to treat chronic health conditions, such as hypertension or depression, may have adverse effects on sperm quality.
How does alcohol consumption affect sperm?
Alcohol consumption can have negative effects on sperm quality and fertility. Excessive alcohol intake can impair hormone production, disrupt sperm production, and decrease sperm motility. Chronic alcohol abuse may also lead to oxidative stress and DNA damage within sperm cells, further impacting fertility.
Is it true that wearing tight underwear can lower sperm count?
Wearing tight underwear, such as briefs or tight-fitting pants, can increase scrotal temperature, which may negatively impact sperm production and quality. Elevated scrotal temperature can hinder sperm production and decrease sperm motility. However, more research is needed to fully understand the long-term effects of tight underwear on sperm count.
Can environmental toxins affect sperm health?
Yes, exposure to environmental toxins can affect sperm health. Toxins such as pesticides, heavy metals, and industrial chemicals can disrupt hormone production, damage sperm DNA, and impair sperm motility. Additionally, exposure to radiation or electromagnetic fields may also have adverse effects on sperm quality and fertility.
What role does genetics play in sperm quality?
Genetics plays a significant role in determining sperm quality and fertility. Genetic factors can influence sperm production, sperm motility, and the overall health of sperm cells. Genetic abnormalities, such as chromosomal abnormalities or mutations in genes related to sperm function, can impact fertility outcomes.
How long can sperm survive in the female reproductive tract?
Sperm can survive in the female reproductive tract for several days, with the ability to remain viable for up to five days under optimal conditions. However, the lifespan of sperm can vary depending on factors such as cervical mucus consistency, pH levels, and the timing of ovulation. Sperm must reach the fallopian tubes within this window to have the best chance of fertilizing an egg.
Can a woman’s fertility affect sperm viability?
Yes, a woman’s fertility can affect sperm viability. Factors such as the quality of cervical mucus, the presence of uterine fibroids or other structural abnormalities, and hormonal imbalances can impact the ability of sperm to reach and fertilize an egg. Additionally, certain medical conditions or treatments that affect a woman’s reproductive health may indirectly affect sperm viability.
Are there any natural supplements that can improve sperm quality?
Yes, several natural supplements may help improve sperm quality and fertility. Supplements such as Coenzyme Q10, L-carnitine, zinc, and vitamin E have been shown to support sperm production, motility, and overall sperm health. However, it’s essential to consult with a healthcare provider before starting any supplements to ensure safety and effectiveness.